Starting the profound and often challenging journey of understanding infertility requires a comprehensive exploration of its intricate facets. Infertility, characterized by the inability to conceive after a designated period of unprotected intercourse, touches the lives of millions globally. This informative article delves into the nuanced landscape of infertility, addressing its types, causes, symptoms, and treatments.

From the intricate interplay of male and female reproductive health to the diagnostic processes and diverse treatment modalities, our aim is to provide a detailed and empathetic guide for those navigating the complexities of infertility. Whether seeking preventive measures, understanding available interventions, or pondering the financial implications, this exploration aims to empower individuals with knowledge, fostering a sense of informed decision-making and resilience on the path to parenthood.
What is Infertility?
Infertility is defined as the inability to conceive after a year of regular unprotected intercourse. It’s crucial to note that fertility issues affect both men and women, emphasizing the need for a comprehensive understanding of the various aspects of infertility.
Types of Infertility:
Infertility manifests in diverse ways, encompassing both biological and situational factors that can affect an individual or a couple’s ability to conceive. Understanding the different types of infertility is crucial for tailoring appropriate interventions.

- Primary Infertility: Primary infertility is diagnosed when a couple experiences difficulty conceiving despite engaging in regular, unprotected intercourse for at least a year. This type is often the initial indication of fertility challenges and prompts individuals to seek medical assistance.
- Secondary Infertility: Secondary infertility arises when individuals who have previously conceived and carried a pregnancy to term encounter difficulties in conceiving again. This form of infertility can be equally emotionally challenging as couples grapple with unexpected hurdles on their fertility journey.
- Female Infertility: Female infertility can stem from various causes, including ovulatory disorders, structural issues in the reproductive organs, or conditions like endometriosis. Understanding the specific factors affecting female fertility is crucial for devising targeted treatment plans.
- Male Infertility: Male infertility is often related to issues such as low sperm count, poor sperm motility, or structural abnormalities in the reproductive organs. Identifying and addressing these factors is essential in optimizing male reproductive health.
- Unexplained Infertility: In some cases, despite thorough medical evaluation, the specific cause of infertility remains elusive. Unexplained infertility is a category where no identifiable issues are found in either partner, making the path to conception more challenging to discern.
- Age-Related Infertility: Age plays a significant role in fertility, particularly for women. As women age, the quantity and quality of eggs diminish, leading to a decline in fertility. Understanding the impact of age is crucial for couples planning to start a family.
- Secondary to Medical Conditions: Certain medical conditions, such as polycystic ovary syndrome (PCOS), diabetes, or autoimmune disorders, can contribute to infertility. Managing these underlying health issues is integral to improving fertility outcomes.
- Lifestyle-Related Infertility: Lifestyle factors, including excessive stress, poor nutrition, smoking, and excessive alcohol consumption, can negatively impact fertility. Addressing these lifestyle factors through modifications and healthier choices can positively influence fertility.
- Genetic Infertility: In some instances, infertility may have a genetic basis. Genetic disorders affecting reproductive organs or the overall reproductive process can lead to challenges in conceiving.
How Common is Infertility?

Infertility is a prevalent and often underestimated issue that impacts a substantial number of individuals and couples worldwide. Contrary to common misconceptions, fertility challenges are not rare, and a deeper exploration into its prevalence sheds light on the scale of this global concern.
- Global Statistics: Approximately 10-15% of couples globally grapple with infertility, highlighting its widespread occurrence. These statistics encompass a broad spectrum of causes, ranging from age-related fertility decline to underlying health conditions affecting reproductive organs.
- Regional Variances: Infertility rates can vary across regions, influenced by factors such as healthcare access, cultural norms, and socioeconomic conditions. In some areas, where access to reproductive healthcare is limited, infertility may be underreported, further emphasizing the need for comprehensive global fertility awareness.
- Age-Related Trends: Age is a significant factor influencing fertility, and as societal trends shift towards delayed parenthood, age-related infertility has become more prominent. Women over the age of 35 may experience challenges in conception due to a decline in the quantity and quality of eggs.
- Male Infertility: While discussions about infertility often focus on female reproductive health, male infertility is also a prevalent concern. Factors such as low sperm count, poor sperm motility, and structural abnormalities in the reproductive organs contribute to fertility challenges in men.
- Psychological Impact: Beyond the statistical figures, it is essential to recognize the profound psychological impact of infertility. The emotional toll on individuals and couples navigating fertility struggles is considerable, emphasizing the need for holistic support systems.
- Changing Dynamics: Societal shifts, including lifestyle changes, increased stress, and environmental factors, contribute to the evolving landscape of infertility. Awareness of these dynamics is vital for both healthcare providers and individuals seeking to understand and address fertility challenges.
- Promoting Open Conversations: Breaking the silence surrounding infertility is crucial for fostering understanding and empathy. Open conversations about fertility challenges help dispel myths, reduce stigma, and encourage individuals to seek timely medical advice.
- Seeking Professional Guidance: Given the prevalence of infertility, it is essential for individuals and couples to approach fertility concerns proactively. Seeking professional guidance early in the journey can improve the chances of successful interventions and increase the range of available options.
Signs of Infertility:

Recognizing the signs of infertility is crucial for individuals and couples who are trying to conceive. While the absence of pregnancy does not necessarily indicate fertility issues, certain signs may warrant attention and prompt the need for a comprehensive fertility evaluation.
- Irregular Menstrual Cycles: Irregular periods can be indicative of ovulatory disorders or hormonal imbalances, affecting the timing of ovulation and conception. Monitoring menstrual cycles and noting irregularities is a key step in identifying potential fertility concerns.
- Painful Intercourse: Pain or discomfort during intercourse, known as dyspareunia, can be a sign of underlying issues such as endometriosis or pelvic inflammatory disease. These conditions may impact fertility and should be addressed with a healthcare professional.
- Hormonal Imbalances: Hormonal irregularities, manifesting as changes in skin, hair, or mood, can affect reproductive health. Conditions like polycystic ovary syndrome (PCOS) can disrupt ovulation, leading to fertility challenges.
- Age-Related Factors: Age is a critical factor in fertility, especially for women. As women age, fertility declines, and women over 35 may experience challenges in conceiving. Being aware of age-related fertility factors is essential for family planning.
- Previous Pregnancy Issues: Individuals who have experienced difficulties carrying a pregnancy to term or have had recurrent miscarriages may be at risk for infertility. Previous reproductive history is an important consideration when assessing fertility concerns.
- Abnormalities in Menstrual Bleeding: Unusual patterns of menstrual bleeding, such as extremely heavy or light periods, may be indicative of underlying issues affecting fertility. Monitoring and discussing these patterns with a healthcare provider is crucial.
- Changes in Libido: A noticeable decrease in libido or sexual desire can be associated with hormonal imbalances or psychological factors, impacting fertility. Open communication about changes in sexual health is essential for addressing potential concerns.
- Issues with Sperm Quality and Quantity: For men, changes in sperm quality and quantity can be a sign of male infertility. Factors such as low sperm count or poor sperm motility may contribute to difficulties in achieving pregnancy.
- Pain or Discomfort in the Pelvic Area: Persistent pain or discomfort in the pelvic region may signal conditions such as endometriosis or pelvic inflammatory disease, both of which can affect fertility. Seeking medical advice for the evaluation of pelvic pain is essential.
- Excessive Stress: Chronic stress can impact reproductive health, affecting hormonal balance and ovulation. Understanding the role of stress in fertility and adopting stress-management techniques may be beneficial for those trying to conceive.
What Causes Infertility?

Infertility can stem from a myriad of factors, both in men and women, contributing to challenges in conception. Understanding these causes is pivotal for targeted interventions and personalized treatment plans. The causes of infertility are diverse, ranging from biological factors to lifestyle choices and underlying health conditions.
- Ovulatory Disorders: Irregular or absent ovulation, a common cause of female infertility, can result from conditions like polycystic ovary syndrome (PCOS) or hormonal imbalances. Disruptions in the ovulatory cycle can hinder the release of mature eggs necessary for fertilization.
- Structural Issues in the Reproductive Organs: Structural abnormalities in the reproductive organs, such as blocked fallopian tubes or uterine abnormalities, can impede the natural flow of eggs and sperm, hindering their meeting for fertilization.
- Endometriosis: Endometriosis is a condition where tissue similar to the lining of the uterus grows outside the uterus. This can lead to inflammation, scarring, and adhesions, affecting the function of reproductive organs and hindering conception.
- Age-Related Decline in Female Fertility: Female fertility diminishes with age, particularly after the age of 35. As women age, the quantity and quality of eggs decrease, making conception more challenging. Advanced maternal age is a significant factor in infertility.
- Low Sperm Count and Quality: Male infertility often results from low sperm count or poor sperm quality. Factors such as hormonal imbalances, genetic factors, or lifestyle choices like smoking and excessive alcohol consumption can contribute to male fertility issues.
- Hormonal Imbalances: Imbalances in hormones crucial for reproduction, such as luteinizing hormone (LH) and follicle-stimulating hormone (FSH), can disrupt the delicate hormonal interplay necessary for ovulation and successful conception.
- Unexplained Infertility: In some cases, despite extensive testing, the specific cause of infertility remains undetermined. Unexplained infertility can be a challenging diagnosis, requiring ongoing exploration and personalized treatment approaches.
- Lifestyle Factors: Certain lifestyle choices can impact fertility. Smoking, excessive alcohol consumption, drug use, and obesity have been linked to fertility issues in both men and women. Adopting a healthier lifestyle may positively influence reproductive health.
- Genetic Factors: Genetic disorders affecting reproductive organs or the overall reproductive process can contribute to infertility. Understanding genetic factors is crucial for couples undergoing fertility evaluations.
- Pelvic Inflammatory Disease (PID): PID, often resulting from untreated sexually transmitted infections (STIs), can cause inflammation and scarring in the reproductive organs, leading to fertility challenges. Early detection and treatment of STIs are essential in preventing PID.
- Psychological Factors: Emotional stress, anxiety, and depression can influence reproductive health. Stress management and emotional well-being are integral components of a holistic approach to fertility.
How is Female Infertility Diagnosed?

Diagnosing female infertility involves a thorough and systematic approach to uncover the underlying factors affecting reproductive health. The diagnostic process aims to identify specific issues related to ovulation, the condition of the reproductive organs, and hormonal imbalances. Here are the key components of the diagnostic journey for female infertility:
- Menstrual History and Ovulation Tracking: Understanding a woman’s menstrual history is a fundamental aspect of infertility diagnosis. Regular and predictable menstrual cycles indicate proper ovulatory function. Tracking ovulation through methods such as temperature charting or ovulation predictor kits provides valuable insights.
- Hormonal Tests: Hormonal imbalances can significantly impact fertility. Blood tests to measure hormone levels, including follicle-stimulating hormone (FSH), luteinizing hormone (LH), thyroid hormones, and anti-Müllerian hormone (AMH), help evaluate the functioning of the reproductive system.
- Imaging Studies: Imaging studies, such as transvaginal ultrasound, provide detailed visualizations of the reproductive organs. This helps identify structural abnormalities, ovarian cysts, or conditions like polycystic ovary syndrome (PCOS).
- Hysterosalpingography (HSG): HSG is a radiologic procedure involving the injection of a contrast dye into the uterus and fallopian tubes. This helps evaluate the patency of the fallopian tubes and identifies any blockages or abnormalities.
- Laparoscopy: In cases where other diagnostic methods do not provide conclusive results, laparoscopy may be recommended. This minimally invasive surgical procedure allows direct visualization of the reproductive organs, facilitating the identification of conditions like endometriosis or pelvic adhesions.
- Ovarian Reserve Testing: Assessing ovarian reserve helps estimate the quantity and quality of a woman’s eggs. Tests such as antral follicle count and AMH levels provide insights into the ovarian reserve, offering valuable information for fertility planning.
- Cervical Mucus Evaluation: The consistency and quality of cervical mucus play a role in fertility. Certain conditions may affect the cervical mucus, hindering sperm mobility. Evaluating cervical mucus can provide additional information during fertility assessments.
- Genetic Testing: Genetic factors can contribute to infertility. Genetic testing may be recommended to identify potential chromosomal abnormalities or hereditary conditions that could impact reproductive health.
- Evaluation of Uterine Structure: Assessing the structure of the uterus is crucial. Conditions such as uterine fibroids or abnormalities may interfere with implantation. Imaging studies and, if necessary, hysteroscopy help in examining the uterine environment.
- Testing for Infections: Infections, especially sexually transmitted infections (STIs), can have adverse effects on reproductive health. Testing for infections and prompt treatment are essential to prevent complications such as pelvic inflammatory disease (PID).
How is Male Infertility Diagnosed?
Diagnosing male infertility is a systematic process that involves a combination of medical history assessment, physical examinations, and various laboratory tests. Identifying the specific factors affecting sperm production, quality, and delivery is crucial for formulating targeted treatment plans. Here are the key components of the diagnostic journey for male infertility:
- Semen Analysis: Semen analysis is a fundamental diagnostic test for male infertility. It evaluates the volume, concentration, motility, and morphology of sperm. A comprehensive analysis provides insights into sperm health and function.
- Hormonal Testing: Hormonal imbalances can impact sperm production. Blood tests measure hormone levels, including testosterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH), helping assess the functioning of the male reproductive system.
- Genetic Testing: Genetic factors can contribute to male infertility. Genetic testing may be recommended to identify chromosomal abnormalities or hereditary conditions that affect sperm production or function.
- Physical Examination: A thorough physical examination of the male reproductive organs helps identify structural abnormalities, such as varicoceles (enlarged veins in the testicles) or blockages in the vas deferens, which can hinder sperm transport.
- Medical History: Understanding the patient’s medical history is crucial. Previous illnesses, surgeries, medications, lifestyle factors, and exposure to environmental toxins can provide valuable information about potential causes of male infertility.
- Post-Ejaculation Urinalysis: A post-ejaculation urinalysis may be conducted to check for the presence of sperm in the urine, which can occur in cases of retrograde ejaculation—a condition where semen enters the bladder instead of being expelled through the penis.
- Ultrasound Imaging: Ultrasound imaging of the testicles and surrounding structures can help identify abnormalities such as varicoceles or blockages. This non-invasive imaging technique provides visual insights into the male reproductive anatomy.
- Testicular Biopsy: In cases where sperm production is severely impaired, a testicular biopsy may be recommended. This involves extracting a small tissue sample from the testicles to assess sperm production and quality.
- Anti-Sperm Antibody Testing: Anti-sperm antibodies can interfere with sperm function. Blood tests can detect the presence of these antibodies, providing insights into immune-related factors affecting fertility.
- Functional Tests: Functional tests, such as the hypo-osmotic swelling test, assess the integrity of sperm cell membranes. These tests provide information about sperm function and their ability to fertilize an egg.
- Scrotal Doppler Ultrasound: This specialized ultrasound assesses blood flow in the testicles and is particularly useful in identifying varicoceles, which can contribute to temperature-related damage to sperm.
How is Infertility Treated?
Addressing infertility often involves a tailored and multidisciplinary approach, taking into account the specific causes identified during the diagnostic process. Treatment options vary, ranging from lifestyle modifications and medications to advanced assisted reproductive technologies (ART). The goal is to optimize fertility and increase the chances of successful conception. Here are the key aspects of infertility treatment:
1. Lifestyle Modifications: For both men and women, adopting a healthy lifestyle can positively impact fertility. This includes maintaining a balanced diet, regular exercise, avoiding tobacco and excessive alcohol consumption, and managing stress. These changes contribute to overall reproductive well-being.
2. Medications: Hormonal medications may be prescribed to address specific issues identified during the diagnostic process. For women, these medications can regulate ovulation, treat hormonal imbalances, or stimulate egg development. For men, medications may enhance sperm production and quality.
3. Surgery: Surgical interventions may be recommended to correct structural abnormalities that contribute to infertility. Procedures such as the repair of blocked fallopian tubes, removal of ovarian cysts, or treatment of varicoceles in men can improve reproductive function.
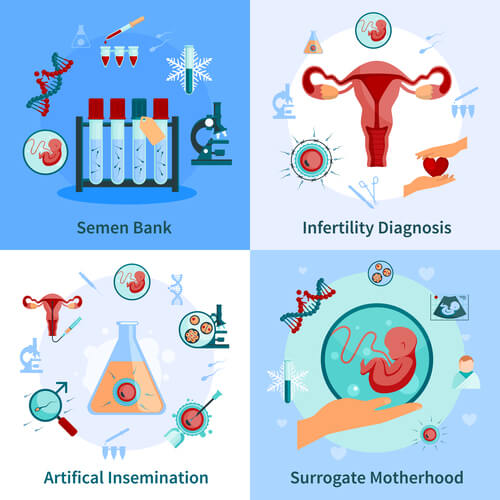
4. Assisted Reproductive Technologies (ART): ART procedures are advanced fertility treatments that involve manipulation of eggs, sperm, or embryos outside the body. Common ART techniques include:
- In Vitro Fertilization (IVF): Involves fertilizing an egg with sperm outside the body and implanting the resulting embryo into the uterus.
- Intracytoplasmic Sperm Injection (ICSI): A specialized form of IVF where a single sperm is directly injected into an egg.
- Intrauterine Insemination (IUI): Involves placing sperm directly into the uterus during the woman’s fertile window.
5. Ovulation Induction: Ovulation-inducing medications may be prescribed to stimulate the ovaries to release eggs. This can be particularly beneficial for women with irregular ovulation or ovulatory disorders.
6. Donor Eggs or Sperm: In cases where one partner has compromised fertility, the use of donor eggs or sperm may be considered. This option is often chosen when a genetic or medical condition makes it challenging to conceive using the individual’s own gametes.
7. Surrogacy: Surrogacy involves another woman carrying and delivering a child for the intended parents. This option is explored when a woman cannot carry a pregnancy to term due to medical reasons.
8. Lifestyle Counseling: Education and counseling play a crucial role in infertility treatment. Understanding the emotional and psychological aspects of fertility challenges can be integral to the overall success of the treatment journey.
9. Pre-implantation Genetic Testing (PGT): PGT is a technique used in conjunction with IVF to screen embryos for genetic abnormalities before implantation. This helps improve the chances of a successful pregnancy and reduces the risk of certain genetic disorders.
10. Donor Embryos: In cases where both partners face infertility challenges, using embryos donated by another couple may be considered as an alternative option for conception.
11. Gestational Carrier: In situations where a woman cannot carry a pregnancy to term, a gestational carrier, who is not genetically related to the child, may be involved in carrying the pregnancy.
Can Infertility be Cured?

The question of whether infertility can be cured is complex and depends on various factors, including the underlying causes, the age of the individuals involved, and the available treatment options. While not all cases of infertility can be “cured” in the traditional sense, significant advancements in reproductive medicine offer a range of interventions that can substantially improve the chances of achieving a successful pregnancy. Here’s a nuanced exploration of the potential outcomes:
- Treatment Success and Pregnancy: Many couples experiencing infertility successfully conceive with the help of fertility treatments. Approaches such as in vitro fertilization (IVF), intrauterine insemination (IUI), ovulation induction, and others have led to countless success stories, enabling individuals to overcome specific fertility challenges.
- Addressing Underlying Causes: In cases where infertility is caused by treatable factors such as hormonal imbalances, structural issues, or infections, addressing these underlying causes can significantly improve reproductive health. Surgical interventions, medications, and lifestyle modifications may contribute to positive outcomes.
- Lifestyle Changes: Adopting a healthier lifestyle through diet, exercise, and stress management can positively impact fertility. For some individuals, lifestyle modifications alone may lead to improved reproductive function and successful conception.
- Advances in Assisted Reproductive Technologies (ART): Assisted reproductive technologies (ART) have revolutionized fertility treatment. While not a cure, these advanced techniques, including IVF and intracytoplasmic sperm injection (ICSI), offer effective ways to bypass certain fertility challenges and facilitate pregnancy.
- Ongoing Research and Innovation: Ongoing research in reproductive medicine continues to uncover new insights and treatment options. Emerging technologies, genetic advancements, and innovative approaches may further expand the possibilities for individuals facing infertility.
- Genetic Screening and Pre-implantation Genetic Testing (PGT): Genetic screening and PGT allow for the identification of embryos with chromosomal abnormalities before implantation. This can enhance the chances of a successful pregnancy and reduce the risk of certain genetic disorders.
- Donor Gametes and Surrogacy: In cases where infertility is insurmountable using one’s own gametes, the use of donor eggs, sperm, or embryos, as well as surrogacy, provides alternative paths to parenthood.
- Emotional Healing: While not a physical cure, emotional healing and support play a crucial role in the fertility journey. Counseling, support groups, and mental health resources can help individuals and couples navigate the emotional challenges associated with infertility.
- Acceptance and Alternative Paths: In some cases, acceptance of the limitations of available treatments and exploration of alternative paths to parenthood, such as adoption or fostering, may be a meaningful and fulfilling choice.
It’s essential to approach the concept of “cure” in the context of infertility with a realistic and individualized perspective. Success in fertility treatments varies, and not all individuals or couples may achieve the desired outcome. Additionally, factors such as age, overall health, and the presence of underlying conditions can influence treatment success.
How Can I Prevent Infertility?
While infertility can result from a combination of biological, genetic, and lifestyle factors, adopting certain practices may contribute to maintaining reproductive health and reducing the risk of fertility challenges. Here are key strategies for individuals and couples interested in proactively preventing infertility:
- Maintain a Healthy Lifestyle: Prioritize a balanced and nutritious diet, ensuring intake of essential vitamins and minerals. Regular exercise and weight management contribute to overall health, positively influencing reproductive function.
- Manage Stress: Chronic stress can impact hormonal balance and disrupt ovulation in women and sperm production in men. Incorporate stress-management techniques such as meditation, yoga, or mindfulness to promote emotional well-being.
- Avoid Smoking and Excessive Alcohol Consumption: Both smoking and excessive alcohol intake have been linked to fertility issues in both men and women. Quitting smoking and moderating alcohol consumption can positively impact reproductive health.
- Practice Safe Sex: Protecting oneself from sexually transmitted infections (STIs) is crucial. STIs can lead to pelvic inflammatory disease (PID) in women, causing damage to reproductive organs. Safe sex practices reduce the risk of STIs.
- Understand Your Menstrual Cycle: Tracking menstrual cycles helps in understanding ovulation patterns, making it easier to identify the fertile window for conception. Knowledge of one’s menstrual cycle is essential for optimizing natural fertility.
- Limit Exposure to Environmental Toxins: Minimize exposure to environmental toxins and pollutants that may impact reproductive health. This includes being mindful of occupational hazards and using protective measures when necessary.
- Address Underlying Health Conditions: Manage and treat existing health conditions promptly. Conditions such as polycystic ovary syndrome (PCOS), diabetes, and thyroid disorders can influence fertility and may require medical attention.
- Avoid Excessive Heat Exposure: For men, prolonged exposure to excessive heat, such as hot tubs or saunas, may negatively impact sperm production. Avoiding prolonged heat exposure to the genital area can help maintain optimal sperm health.
- Consider Genetic Counseling: For individuals with a family history of genetic disorders or those with known genetic conditions, seeking genetic counseling can provide insights into potential risks and guide family planning decisions.
- Age Awareness: Women should be aware of age-related fertility decline. As women age, the quantity and quality of eggs decrease, impacting fertility. Considering family planning earlier can be beneficial in optimizing fertility.
- Folic Acid Supplementation: Women planning to conceive are often advised to take folic acid supplements. Adequate folic acid intake before and during early pregnancy can reduce the risk of certain birth defects.
- Regular Health Check-ups: Routine health check-ups allow for the early detection and management of conditions that may affect reproductive health. Regular gynecological and urological examinations are essential for preventive care.
- Balanced Sexual Activity: While attempting to conceive, maintaining a balanced approach to sexual activity is important. Avoiding extremes, such as excessive or infrequent intercourse, can support natural fertility.
- Seek Timely Medical Advice: If concerns arise or if conception is taking longer than expected, seeking timely medical advice is crucial. Early intervention can identify and address potential fertility issues.
It’s important to recognize that while these strategies can contribute to overall reproductive well-being, fertility is influenced by a combination of factors, and not all cases of infertility can be prevented. Consulting with healthcare professionals and the best IVF center in Indore provides personalized guidance based on individual health profiles and goals for family planning.
What Can I Expect if I Have Infertility?
Facing infertility can be an emotionally challenging and complex journey, and individuals or couples navigating this path often encounter a range of physical, emotional, and practical considerations. Here is an exploration of what one can expect when dealing with infertility:
- Emotional Rollercoaster: Infertility often brings about a range of emotions, including sadness, frustration, anxiety, and even grief. It’s essential to acknowledge and express these feelings and consider seeking emotional support from partners, friends, family, or mental health professionals.
- Medical Evaluation: Upon recognizing fertility concerns, the first step typically involves a thorough medical evaluation. Both partners may undergo various tests, including hormonal assessments, imaging studies, and genetic testing to identify potential causes of infertility.
- Specialized Fertility Consultations: Consultations with fertility specialists or reproductive endocrinologists may be recommended. These specialists guide individuals or couples through the diagnostic process, explain treatment options, and develop personalized plans based on the identified causes of infertility.
- Treatment Options: Depending on the diagnosis, individuals can expect discussions about various treatment options. These may include lifestyle modifications, medications, surgery, assisted reproductive technologies (ART) such as in vitro fertilization (IVF), or alternative paths to parenthood, such as surrogacy or adoption.
- Financial Considerations: Infertility treatments often involve financial considerations, and individuals may need to navigate the costs associated with diagnostic tests, treatments, and possible assisted reproductive technologies. Understanding insurance coverage and exploring financial assistance options is part of the process.
- Lifestyle Adjustments: Depending on the treatment plan, individuals and couples may need to make lifestyle adjustments. This could include dietary changes, the incorporation of medications, and adhering to specific protocols associated with fertility treatments.
- Uncertainty and Patience: Infertility treatment outcomes can be uncertain, and success is not guaranteed. Patience becomes a crucial aspect of the journey as individuals may need to undergo multiple treatment cycles, each with its own set of emotional and physical challenges.
- Support Networks: Establishing a robust support network is vital. This may involve joining support groups, seeking counseling, or connecting with others who have experienced or are experiencing infertility. Sharing experiences and gaining insights from those who understand can provide valuable emotional support.
- Coping with Setbacks: Not every treatment cycle may result in success, and setbacks are a common part of the infertility journey. Learning to cope with disappointments, adjusting expectations, and exploring new approaches may become necessary.
- Decision-Making and Family Planning: Infertility prompts individuals and couples to make challenging decisions about family planning. Choices may include whether to pursue further treatments, consider alternative family-building options, or embrace a child-free lifestyle. Open communication and alignment in decision-making are crucial.
- Personal Growth: While navigating the complexities of infertility, individuals often experience personal growth. This can involve developing resilience, acquiring coping strategies, and gaining a deeper understanding of oneself and one’s priorities.
- Celebrating Successes: Celebrating small victories and recognizing the courage it takes to face infertility is important. Successes may include progress in treatment, personal achievements in coping, or finding new paths to parenthood.
It’s essential to approach the journey with a compassionate and patient mindset. Infertility is a unique and individual experience, and the process can vary for each person or couple. Seeking information, building a support system, and maintaining open communication with healthcare professionals are crucial steps in navigating the challenges and uncertainties associated with infertility.
Does Insurance Cover Infertility Treatment?
Insurance coverage for infertility treatment varies widely and is contingent on factors such as the specific insurance plan, geographic location, and the underlying causes of infertility. While some insurance plans may offer partial coverage for diagnostic tests, consultations, and certain fertility treatments, others may provide more comprehensive coverage.
Typically, assisted reproductive technologies (ART) such as in vitro fertilization (IVF) may have limited coverage or may not be covered at all. It is crucial for individuals or couples facing infertility to thoroughly review their insurance policies, understand the scope of coverage, and explore potential out-of-pocket expenses. Engaging in open communication with insurance providers and seeking clarification on coverage details can help individuals make informed decisions about their fertility treatment options while managing associated costs.
Ending Notes:
In the pursuit of parenthood amidst fertility challenges, it’s paramount to recognize that the journey is as unique as the individuals undertaking it. Infertility may present unforeseen hurdles, but it does not define the capacity to become parents. The resilience exhibited in navigating this complex path is a testament to unwavering determination and boundless love. Embracing the possibility of alternative routes to parenthood, seeking support from a network of understanding individuals, and staying informed about evolving fertility treatments can be empowering.
Parenthood, in all its forms, is a testament to the enduring strength of the human spirit. As you embark on this transformative journey, remember that the love, commitment, and courage you bring to the process are the very qualities that make parenthood a remarkable and awe-inspiring adventure.
FAQs:
Infertility is the inability to conceive after a year of regular, unprotected intercourse.
Approximately 10-15% of couples globally experience infertility.
Causes include ovulatory disorders, structural issues, endometriosis, age-related factors, and hormonal imbalances.
Male infertility may result from low sperm count, poor sperm quality, hormonal imbalances, or structural issues.
Diagnosis involves menstrual history, hormonal tests, imaging studies, and, if necessary, procedures like hysterosalpingography or laparoscopy.
Diagnosis includes semen analysis, hormonal tests, genetic testing, physical examination, and, if needed, imaging studies.
While not always “cured,” infertility can often be treated successfully with lifestyle changes, medications, surgery, or assisted reproductive technologies.
Treatments range from lifestyle modifications and medications to assisted reproductive technologies (ART) such as in vitro fertilization (IVF) and surrogacy.
Maintain a healthy lifestyle, manage stress, avoid smoking and excessive alcohol, practice safe sex, and seek timely medical advice.
Individuals can expect emotional challenges, medical evaluations, discussions about treatment options, financial considerations, and the possibility of alternative paths to parenthood.










